Annamaria's First ASCO Annual Meeting
Five days that changed how she sees her role as a patient advocate
Author: Annamaria Scaccia (COA Board Member)
If there's one word to describe my first ASCO experience, it's "bridge."
Last month, I attended the 2025 American Society of Clinical Oncology Annual Meeting as a Patient Advocate Scholarship recipient, representing the Chromophobe and Oncocytic Alliance (COA). Every year, tens of thousands of cancer professionals gather to share the latest research and shape the future of cancer care. Patient advocates join them—not as observers, but as bridges who connect new science to the people who need it most.
I joined Katie Coleman, COA’s founder, and Laura Esfeller, a fellow board member, at ASCO to stay informed about current chromophobe RCC research for our nonprofit work. But while there, we also took in the bigger picture. We connected with oncologists, engaged with other advocates, and learned to ask the right questions about what we know, what we're missing, and how to close the gaps.
While I didn't leave with all the answers, I left with something more valuable.
Clarity.
I'm not a spokesperson or thought leader. But I am a bridge—between science and patients, between research and application, between expertise and curiosity.
Here’s how my time at ASCO unfolded.
Imposter syndrome in knock-off Birkenstocks
Technically, I was prepared for ASCO. I downloaded the app, synced my agenda, mapped directions. I knew where I needed to be. But once I arrived at McCormick Place, I felt out of my depth immediately.
There I was, surrounded by over 40,000 oncologists, my knock-off Birkenstocks squeaking against the polished floor as I made my way to pick up materials for the next day. Everyone else looked like they belonged—suits, lanyards, self-assured handshakes. I wondered if my tattoos and lounge set screamed "patient advocate scholarship recipient" or just "lost."
For all my advocacy work, I still felt like three children hiding in a trench coat who somehow infiltrated the adults. The imposter syndrome was loud—loud while standing in line for coffee, overhearing researchers drop scientific terms I needed to Google. Loud while playing third wheel in conversations about new medications I'd never heard of.
That's when I realized I wasn't there to pretend I belonged. I was there to learn, and my questions—even the most basic ones—mattered.
Instead of spiraling, I decided to focus on what this was: a weekend to learn, to build community, and to finally meet people I'd only known through a screen.
Sometimes, being the outsider is exactly who you need to be—even at the world's largest cancer conference. And day 2 reminded me why this perspective is needed in patient advocacy.
When joy becomes resistance
So much happened on Day 2—the science, the breakthroughs, the hallway conversations, the therapy dogs. But the moment I keep returning to is the Celebration of Queer Joy, organized by Fight CRC, Cheeky Charity, and the National LGBT Cancer Network.
My chromophobe journey didn't directly intersect with this moment, but what happened on National Cancer Survivors Day brought to light what healthcare often overlooks: LGBTQIA+ visibility. It reminded the world that we can—and should—use our patient advocacy to celebrate both queer joy and cancer survivorship together.
Because the statistics are stark. The existing systems don’t empower our inclusion in research, in guidelines, or in medical practice. How many clinical trials ask about sexual orientation or gender identity? How many oncologists understand the unique challenges transgender patients face during treatment?
Still, here we were—surviving systems not built for us, advocating and refusing to disappear. The joy we celebrated was our commitment to be seen.
I watched cancer survivors who, for decades, have fought for inclusion embrace newcomers like me. With my "Save the Booties" flag and rainbow butt cheek heart pin, I found my place in a community that won’t stay invisible.
Representation in cancer care saves lives—whether for rare cancers like chromophobe RCC or for communities like LGBTQIA+ patients. When these voices are in the room, at the table, on the podium, and in the data, patients get better care, outcomes improve, and the system works better. This is why I tell stories for a living—to be heard and to be visible.
As I was finding my footing, Day 3 brought a different kind of challenge—one I hadn't expected.
The identity crisis no one talks about
Nearly five years into survivorship, and I’m still asking: Who am I as a patient advocate?
For the first two years of survivorship, I was known as the "one-kidney bodybuilder," proving that life after cancer doesn't have to shrink when you lose an organ. That story felt empowering—until thyroid cancer arrived and triggered an identity crisis.
Between fall 2020 and summer 2023, I lost my left kidney, lost my thyroid, and became a double cancer survivor. Then by late 2024, I was diagnosed with a precancerous polyp, putting me at risk for a third primary cancer. No mutation. No family history. Just more uncertainty.
The weight of multiple diagnoses has taught me that uncertainty is both personal and scientific. Throughout ASCO, I heard researchers grappling with similar questions: How do we treat cancers that don’t respond to standard immunotherapies? How do we identify which patients might best benefit from combination therapies? How do we take advantage of novel research to predict treatment response?
Sitting in those sessions, I realized I’ve been wrestling with the same discomfort that drives scientific discovery—the space between what was and what might be. Maybe that’s exactly where I need to be.
The truth is, I’ve been clinging to an identity that no longer fits because it’s easier than facing what comes next. But I don’t belong to just one experience anymore. I’ve outgrown that story.
“You are where you’re supposed to be.”
I’ve learned so much from the people I’ve met—and even more from those I’m still getting to know. Katie, Laura, and so many other patient advocates helped me open doors while I’m still figuring out what room I’m in.
At one point, I shared with a metastatic breast cancer survivor that I wasn’t sure where I fit. She responded with something I’ve been holding onto ever since: “You are where you’re supposed to be.”
I still feel like I’m behind sometimes. Like I should already know who I am and what my purpose is. But maybe this uncertainty is part of the process. Maybe not fitting perfectly means I’m still growing. Maybe being in between is an opening.
The next day, while waiting to head back home to Austin, I had a text conversation with Katie that helped crystallize something I'd been feeling throughout the conference.
We went back and forth about how we felt as advocates and where we fit in this space. "It's okay if it takes a bit to figure out where you want to point [your impact]," Katie wrote to me. "Because it's not your story that makes an impact, it's you."
The impact I want to make is through bridging science and survivorship. And nowhere is that bridge needed more than in rare cancers like chromophobe RCC.
The science that could change everything
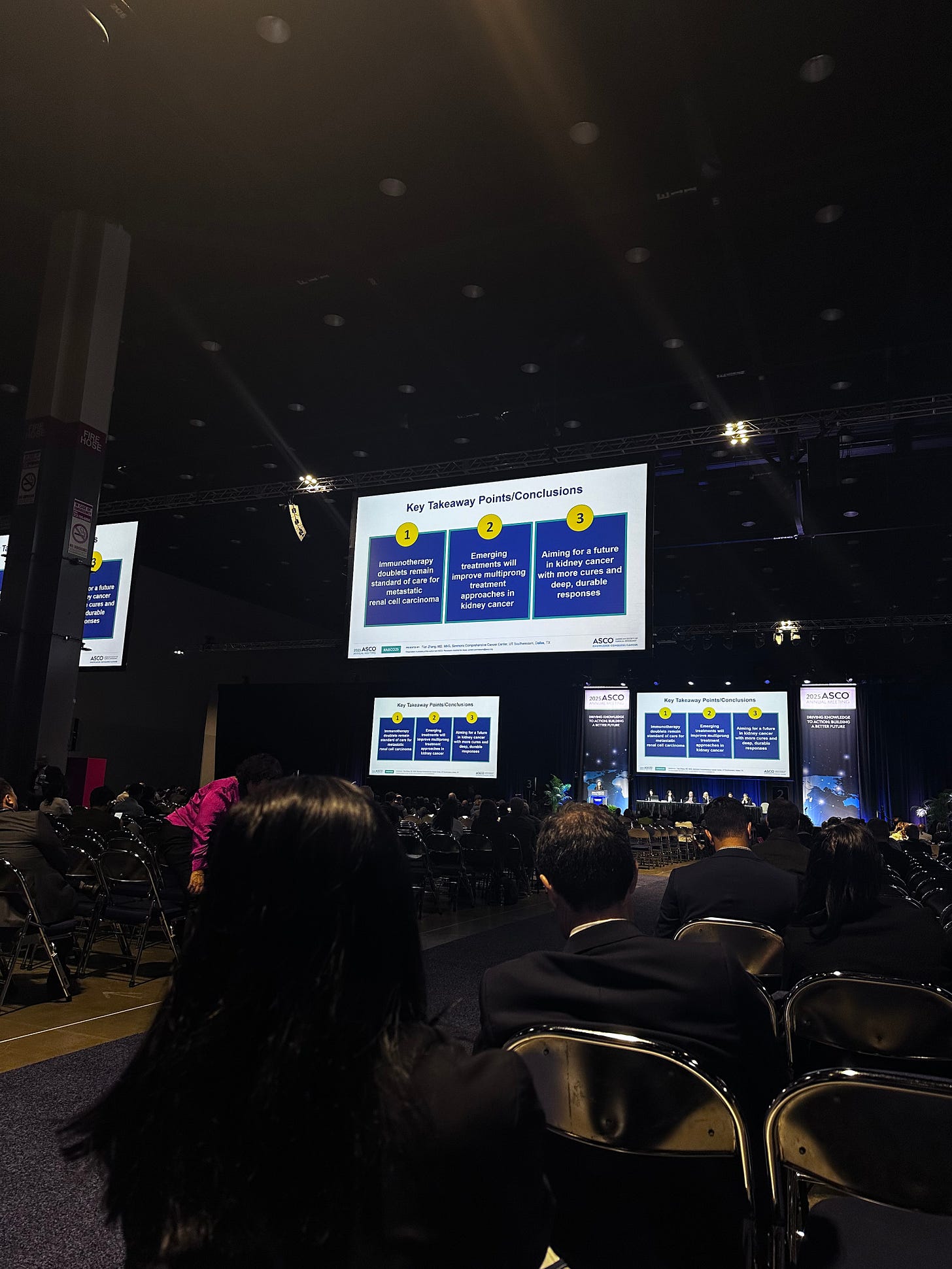
At ASCO, I watched presentations about promising combination therapies, novel biomarkers, and personalized treatments. Almost all of them focused on clear cell RCC, the most common subtype.
Diving into the abstracts I'd missed, I found breadcrumbs that could matter for the chromophobe kidney cancer community. Researchers are exploring if combination therapy works better than single agent treatments—even for kidney cancers like chRCC, which don't typically respond to immunotherapy. Blood tests are being explored to help predict which patients might benefit from specific treatments. And how the gut microbiome can affect how well immunotherapy works. The gut microbiome is an area of growing interest across healthcare as groups explore both the impact diet and exercise may have as well as biotherapeutics such CBM588 which is currently being explored in kidney cancer.
These abstract findings are roadmaps for the studies our chromophobe community needs. We need researchers to test these approaches specifically in chromophobe patients. We need biomarker studies that include our cancer type. We need clinical trials that will turn these promising directions into treatment options tailored to the biology of chromophobe.
I didn't leave ASCO with a perfect path forward, but I did leave with clarity about what I'm here to do. I am here to translate, to connect, and to open space. I am here to make research feel human and make lived experience visible in rooms where it's often missing.
I hope to continue this work as a COA board member, supporting our chromophobe kidney cancer community as we push for more research, visibility, and inclusion—while bridging connections with other cancer communities facing similar challenges and promises.
If you're part of a rare cancer community, you know we're used to being footnotes in research and afterthoughts in clinical trials. What if we stopped waiting for others to include us and started rallying together to support the studies we need?
What if we all became the bridge?
Annamaria Scaccia
Annamaria Scaccia is a poet, essayist, and award-winning journalist who has survived both kidney and thyroid cancer by the age of 40. She uses her experiences to support other survivors through education, awareness, and fundraising initiatives. Annamaria also hosts Kidney Cancer Unfiltered, a podcast from the Kidney Cancer Association, a COA affiliate partner. Outside of work, she’s a one-kidney bodybuilder, a self described coffee snob, and someone who would never turn down a good loaf of bread. Originally from Brooklyn, Annamaria now lives in Austin with her son, her partner, and their two dogs and two cats.